PROCAS and BC-PREDICT
Predicting the Risk of Cancer at Screening
For women, individual breast cancer risk is highly variable, and yet the interval of mammograms in the NHS Breast Screening Programme (NHSBSP) is every three years, regardless of individual risk. However, evidence suggests that around 10% of women at screening age (50-74), without a significant family history of breast cancer, are likely to be at moderate or high risk of breast cancer according to guidance published by NICE in 2013. This may be due in part to certain lifestyle factors and other factors such as breast density.
To investigate how risk scores could be implemented in the NHS, PROCAS 1 (Predicting the Risk of Cancer at Screening) highlighted a need to collect risk information from women to create a better tailored breast screening programme that currently exists.
We speak to Professor Gareth Evans about how the findings from PROCAS 1 led to the inception of PROCAS 2, which assesses the feasibility of implementing a personalised risk score into a woman’s first screening appointment and the associated impact on NHS staff, patients and other related organisations.
PROCAS 1
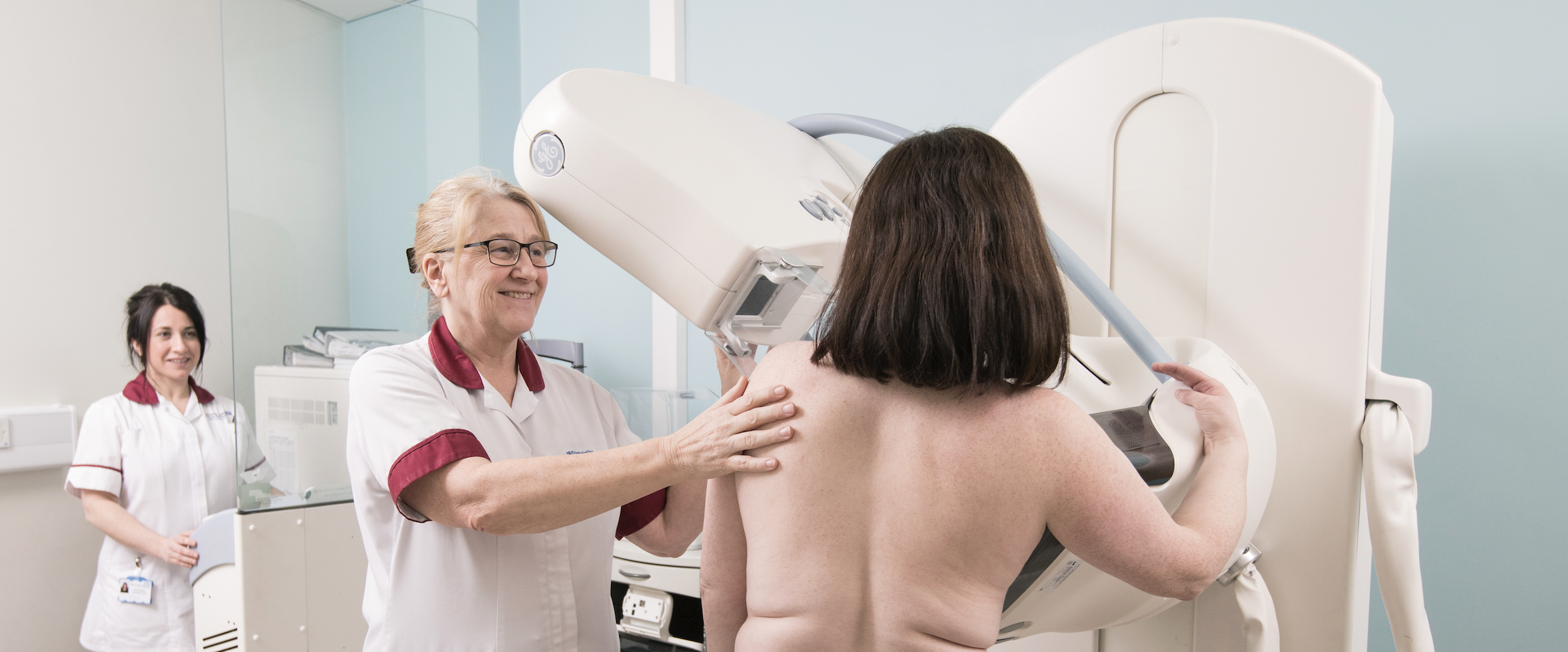
In 2009, PROCAS 1 was launched as the largest recruiting research study in the UK, involving 57,900 women over six years. Led by Professor Gareth Evans, this study involved women attending their first mammogram within Greater Manchester. It gathered additional details such their current health, age at first period, age at first pregnancy, age at menopause, HRT use, diet, BMI and weight gain, and lifestyle choices. From this information, a breast cancer risk score was determined that estimated each woman’s risk of developing the disease in the next ten years. Researchers also looked at the breast density from mammograms, as greater breast density can increase the risk of an individual developing breast cancer by up to six times.
As part of the study, 10,000 women were selected for collection of DNA through a saliva sample which then contributed towards calculating a polygenic risk score, an even more accurate but more costly way of assessing breast cancer risk.
Results showed that 94% of women who were recruited wanted to know their risk score and thus, the study acted to highlight the need for a more tailored breast screening programme within the NHS. Additionally, further research indicates that women who were informed that they were at high risk were more likely than those not informed to take up preventative medication to reduce their risk of developing breast cancer.
However, with a number of unknowns around the implementation such as effects on the NHS workforce of a breast screening programme such as that used in PROCAS 1, this programme needed to be implemented in a practical setting to assess its feasibility. This would show if this screening method could be done in real-time and show if risk feedback could be provided in a meaningful way within a critical time window.
PROCAS 2
Following from PROCAS 1, 2017 saw the inception of PROCAS 2, co-led by Professor Gareth Evans and Professor David French. This project ran for three years to assess the feasibility of offering a personalised risk score at a woman’s first breast screening appointment. This second stage also evaluated the impact of such an implementation on the workforce and patients as well as the health psychology and economic feasibility.
Based on learnings from PROCAS 1, this new study theorised that risk stratification as part of the NHSBSP should produce a better balance of benefits and harms. The main benefit being NICE approved increased frequency of screening and chemoprevention for women who were previously unaware they had an increased risk of breast cancer.
PROCAS 2 also looked into key potential harms of implementation such as increased anxiety found in women receiving their breast cancer risk scores. Additionally, it assessed the economic feasibility of implementation through a decision-analytic model-based cost-effectiveness analysis.
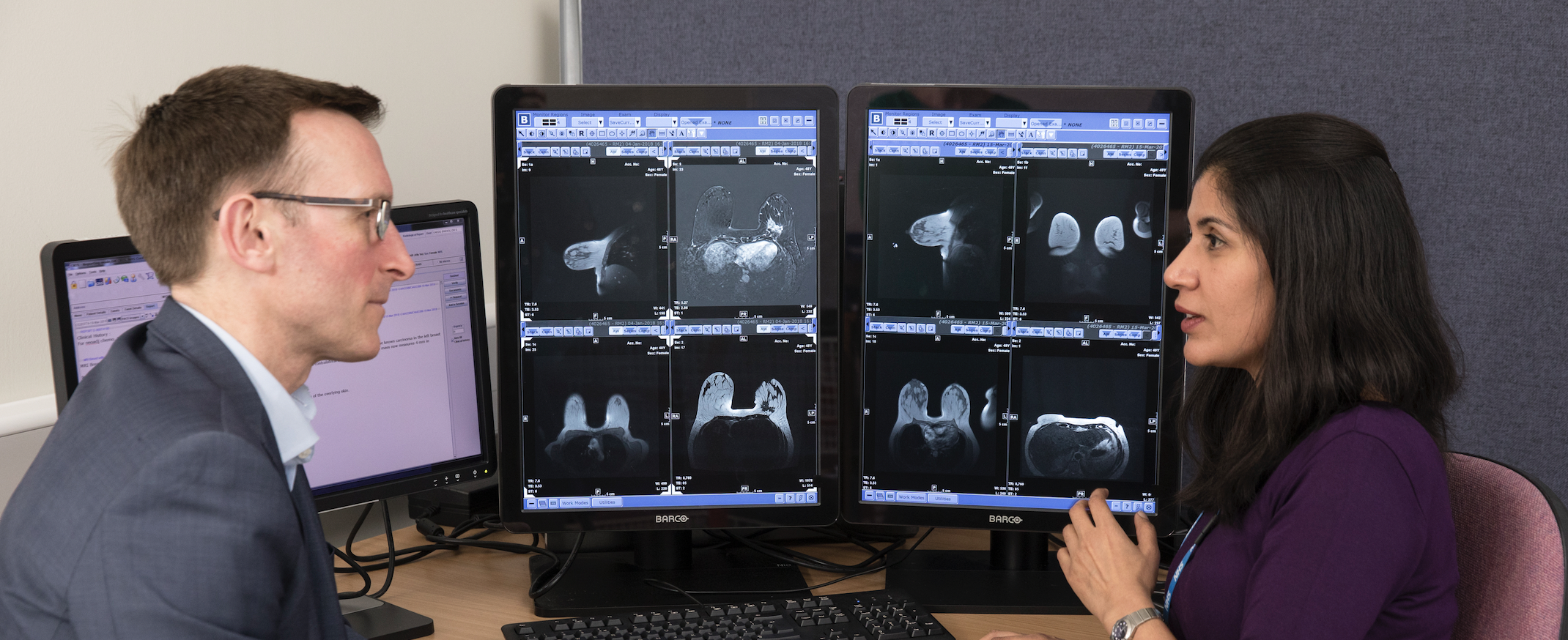
The researchers developed BC-Predict as part of this study which collected information on women’s risk factors when invited to NHSBSP. BC-Predict then produced feedback letters which invited women at high risk or moderate risk to a discussion with a family history or risk and prevention clinic to discuss prevention and early detection.
The study recruited and gathered feedback from 3,000 women of 18,000 invited. It comprised a non-randomised fully counterbalanced study design which included approximately equal numbers of women offered NHSBSP and BC-Predict. The team worked to develop a digital platform with CRA Health so that the women could enter their information that would feed into a risk score digitally. The team also designed a way of assessing mammograms of the women with the . This information was then collated and added to CRA Health database.
Women were then provided with a ten-year breast cancer risk, which was categorised as follows: below average, average, above average, high risk. These women subsequently received recommendations detailing a summary of their risk category and next steps. Women in ‘above average’ or ‘high risk’ categories were informed they could make a subsequent appointment with a healthcare professional for further discussions. The team then assessed potential benefits of women receiving this information such as uptake of risk consultations, additional screening and chemoprevention.
Read more about the assessment of the benefits and harms of risk stratified screening as part of the NHS Breast Screening Programme in our other impact case study.
Results of PROCAS 2
In reviewing the uptake of risk appointments, preventative medication and additional screening of women identified at ‘above average’ or ‘high risk’, who attended risk appointments showed that 77% of women went on to using preventative medicine to reduce their risk of developing breast cancer. PROCAS 2 highlighted that identifying women as ‘above average’ or ‘high risk’ was successful in both encouraging high-risk women to take preventative medication, halving their risk of women developing breast cancer, and showing that BC-Predict is also cost saving to the health service in preventing cancer development. Thus, PROCAS 2 concluded that risk stratification in an NHS setting was feasible, acceptable and that women were inclined to act on their risk information.
Next steps
After holding a consensus conference, the PROCAS 2 research team are currently assessing their findings and constructing a plan for the future. The team will then proceed to discuss this with the UK National Screening Committee to see if they would like further research such as a randomised control trial, or additional information around low-risk women to see about the feasibility of reducing screening intervals.
MyPeBS and WISDOM are two current clinical trials looking at the feasibility of four-yearly screening in ‘low-risk’ women. These trials could feed into the decision-making process of the Screening Committee.
Useful resources
PROCAS 1 programme report: https://www.ncbi.nlm.nih.gov/books/NBK379493/
BC-Predict study protocol: https://pubmed.ncbi.nlm.nih.gov/32552763/
Further information: https://preventbreastcancer.org.uk/breast-cancer-research/research-projects/early-detection-screening/procas/



