PROCAS 2
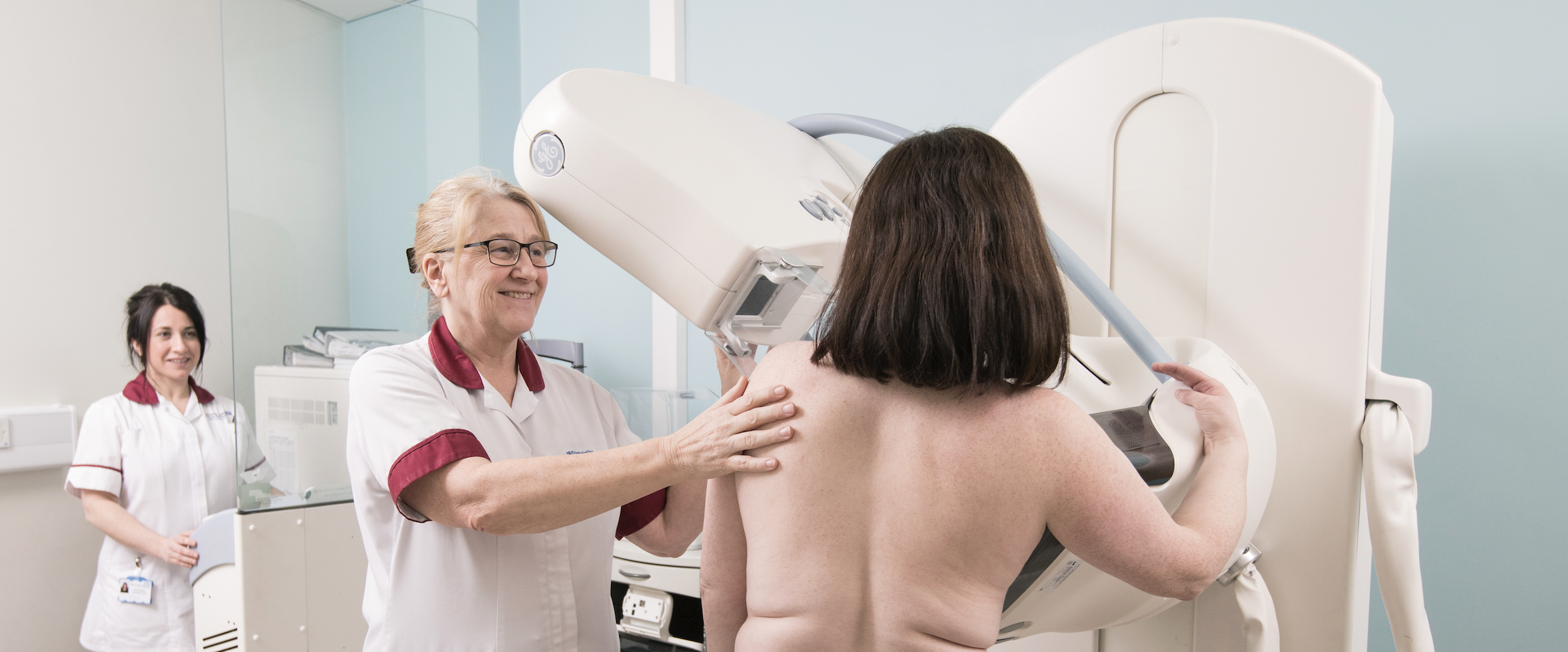
Assessing the benefits and harms of risk stratified screening as part of the NHS Breast Screening Programme

PROCAS 1, led by Professor Gareth Evans, was launched in 2009 as the largest recruiting research study in the UK, comprised of 57,000 women. This study involved women attending their first mammogram in Greater Manchester where it gathered additional details of factors that contribute to breast cancer risk, as well as breast density recordings. From these factors, the study generated breast cancer risk scores, classifying women as ‘below average’, ‘average’, ‘above average’ and ‘high risk’.
Those women classified as ‘above average’ or ‘high risk’ were informed they could make a subsequent appointment for further discussion around measures such as additional screening and chemoprevention. This study highlighted the importance of embedding risk stratification and tailored screening for breast cancer within the NHS Breast Screening Programme (NHSBSP), with 94% of women wanting to know their personal risk score.
The second stage of this project, PROCAS 2, which was co-led by Professor Gareth Evans and Professor David French, was launched in 2017 and ran for five years. A key aim was to assess the feasibility of implementing the risk stratification programme used in PROCAS 1, into a routine NHS setting. The research considered balances of benefits and harms of the programme, called BC-Predict. Harms considered were those such as potential increased anxiety of the women who participated, the effects on NHS staff, increased cost for little health benefit and increased workload for healthcare staff embedding BC-Predict into NHSBSP.
We speak to David French, Professor of Health Psychology about his research around effects on the NHS workforce of embedding BC-Predict into NHSBSP, assessing the psychological effects of women enrolled on BC-Predict and the focus of PROCAS 2 in addressing health inequalities.
When implementing any new screening process such as BC-Predict, it is important to assess the changes to a health care system and ensure that there is no distress caused to the patients, and that the workforce can safely and effectively implement any new screening practices.
Professor David French
Professor of Health Psychology, The University of Manchester
Understanding the acceptability of BC-Predict
Implementing BC-predict within the NHSBSP involves evaluating a series of potential benefits and harms. Key potential benefits include a greater uptake of risk consultations, additional screening, offering drugs that can reduce the risk of breast cancer and health behaviour changes for ‘above average’ or ‘high risk’ women. Conversely, implementing BC-Predict could contribute to an increased workload for the NHS workforce with some healthcare professionals concerned that BC-Predict would cause excess work and it was therefore imperative that PROCAS2 acted to assess any strain on the NHS workforce.
In addition, as BC-Predict acts to risk stratify women, it was also feared that those women who received risk scores of ‘above average’ or ‘high risk’ would experience elevated and maintained levels of general anxiety and cancer worry around a potential cancer diagnosis, while also presenting the potential threat that those identified as ‘below average’ or ‘average’ would see them disengaging from regular screening.
As a result, qualitative and questionnaire-based work was carried out as part of PROCAS 2 to understand the key issues behind the successful implementation of BC-Predict into NHSBSP.
Methods of assessment
To assess the effects on the NHS workforce, researchers ran one-to-one interviews with NHSBSP healthcare staff to provide insight into capacity issues within the NHS as well as an indication of the training and support required to deliver BC-Predict on a larger scale. Additionally, working groups of service users provided continuous feedback to the team around any issues they were experiencing around the implementation of BC-Predict.
To understand the effects of implementing risk stratified screening on women, the researchers focused on a comparison of women offered the standard NHS Breast Screening Programme (NHSBSP) and those on BC-Predict, the screening programme within PROCAS 2.
Levels of anxiety and worry around cancer were obtained through self-report questionnaires. All women completed questionnaires at the time of their first mammogram to obtain baseline recordings of anxiety and worry. Subsequently, some ‘below average’ and ‘average’ risk women were invited for an interview one month after receiving their risk feedback letter, while some women at ‘above average’ or ‘high risk’ were interviewed six months after this letter, giving them sufficient time to explore screening options or preventative medications.
Results
The work with NHS healthcare staff provided insight into capacity issues and indication of the training and support required. In brief, the additional workload was less than was anticipated, although this was still of concern to people working within an already stretched NHS. Any future rollout needs to ensure that there is adequate staffing to support such an innovation, as well as being appropriately trained to answer questions.
Through the interviews with women on each screening programme, no evidence was found of any prolonged increase in anxiety or cancer worry. Through comparing both the baseline and subsequent interviews, this acted to conclusively show that the implementation of BC-Predict into NHSBSP had no adverse lasting psychological distress and thus this should not act as a barrier to implementation.
Addressing health inequalities
To address screening uptake in a group that has previously seen low take up, PROCAS 2 researchers interviewed British Pakistani women in East Lancashire. The aim of these interviews was to focus on an underserved population and develop materials that would improve understanding of how to reach these seldom heard communities.
This work with British Pakistani women has led to improvements within the breast screening programme in Greater Manchester, seeing a change in screening materials such as including multiple language translations along with better signposting to this material.
Additionally, PROCAS 2 placed further efforts on engaging women from other ethnic minority groups. Notably, PROCAS 2 included a patient advisory group which involved a varied group of ethnic minority women. These women contributed to discussions around improving screening materials for breast cancer as well as helping to develop ways of encouraging take up in these communities.
The researchers concluded that more community outreach work is required to engage ethnic minority groups and thus increase their uptake in screening as well as programmes such as BC-Predict. However, the approach taken seemed to work well in reaching these women.
Next steps
Following on from the findings of PROCAS 2, David and the research team held a consensus meeting to focus on the implications of findings, and discussions around feasibility and what more needs to be done to effectively implement BC-Predict into the NHSBSP and to identify and address any uncertainties which are still remaining.
The team are collating findings from the consensus discussion to present to the NIHR and proceed with discussions with the UK National Screening Committee to see if they would like further research to address any remaining uncertainties, or additional information around whether it is a good idea to recommend to low-risk women that they reduce screening intervals.