Penile cancer
Changing the management of Lymph Node-positive Penile Cancer
A systematic review examining the clinical evidence for lymph node-positive penile cancer has led to changes in treatment guidelines and an Impact Award for the team. The international team led by researchers at The Christie and The University of Manchester examined more than 3000 abstracts involving more than 100 studies to identify ways to improve survival in this rare cancer.
“Our synthesis of existing evidence in this rare condition offers valuable insights into the most effective treatment strategies for advanced penile cancer, while minimizing side effects when surgery alone might be curative. We are delighted to witness this truly collaborative global effort shaping international guidelines for this debilitating condition. It is evident that there is a pressing need for greater awareness and further research to enhance early detection and treatment of penile cancer. Manchester is exceptionally well-positioned to contribute significantly to this endeavour.”
Dr Ashwin Sachdeva | NIHR Academic Clinical Lecturer in Urology, University of Manchester & Consultant Urological Surgeon, The Christie Hospital – Lead author
What is penile cancer?
Penile cancer is a rare cancer that mostly affects the skin of the penis and the foreskin. It has an incidence of 0.5-1 in 100,000 males and has good survival rates when it is confined within the organ. However, unfortunately one-third of penile cancer cases will have metastases that have spread into the inguinopelvic lymph nodes (LNs) (inguinal (groin) and pelvic nodes) at the time of presentation, which is associated with poor survival. This is classified as ‘Lymph Node-metastatic penile cancer’.
The survival for LN metastatic penile cancer is approximately 50% at three years which drops to 30% at five years, with higher levels of nodal disease or spread to other organs (such as lungs, liver, bones and brain) being associated with worse outcomes.
Early diagnosis and management of LN involvement in penile cancer, alongside multimodal treatment approaches in advanced disease, can significantly improve survival.
What are some of the challenges with penile cancer?
Penile cancer can often be considered as having a more significant impact on quality of life (QoL) than other more widely discussed cancers, due to its stigmatisation. Patients have reported that they not only suffer the psychological and emotional stress of a cancer diagnosis but also the psychological impact and stigma of cancer on an intimate part of the body.
Current treatment regimens can also cause significant physical and emotional changes to a patient, thereby resulting in feelings of mutilation, loss of masculinity and coping with the impact on voiding and sexual function. In turn, this can result in breakdown in relationships and withdrawal from society. Additionally, long-term management of side-effects of treatment, such as lymphoedema (swelling of the legs), also presents a significant challenge for many of these men.
Although penile cancer mainly affects men over the age of 50-years-old it can appear in patients younger than this and sadly, many patients each year present with late-stage cancer. This is due to several factors including a lack of awareness of penile cancer in the general population and amongst healthcare professionals, as well as fears regarding treatment and stigmatisation. It is not uncommon for men to ignore symptoms for up to six to nine months before presenting to their GP.
Most commonly, penile cancer presents as a lump or sore on the surface of the skin and can have a discharge or bleed. In men with tight foreskins this can often hide the lump as they are unable to pull the foreskin back to examine themselves. In some circumstances men may also develop a lump in the groin as well.
“Most men aren’t aware that penile cancer exists until they are diagnosed with it. From that moment on their lives and the lives of those closest to them change. Most men undergo surgery to their penis as well as groins, which challenges their own perceptions of themselves, and can have lifelong effects both physically and psychologically. The rare nature of the disease makes research and improvements in diagnostic, and treatment challenging. This important study highlights the most effective treatment strategies for advanced penile cancer and acts as a clarion call to patients, providers and research groups to develop national and international networks.”
Mr Arie Parnham | Consultant Urologist, The Christie Hospital

Management of penile cancer with current standards of care
Penile cancer is currently managed in two parts: Management of the primary tumour and management of the lymph nodes in the groins and pelvis.
Penile cancer is a rare type of cancer that affects the penis, often beginning in the skin cells before spreading to deeper tissues. The management of penile cancer involves two main aspects: treating the primary tumour in the penis itself and addressing the cancer’s spread to nearby lymph nodes, particularly those in the groin and pelvic areas.
The first step usually focuses on removing or treating the primary tumour, which might involve surgery, radiation, or other therapies aimed at eliminating the cancerous cells in the penis.
The second crucial aspect of treatment is managing the lymph nodes, which are small, bean-shaped structures that play a key role in the body’s immune system. Cancer can spread to these lymph nodes, particularly those in the groin and pelvis, which then become sites for further disease. When cancer has spread to these lymph nodes, a procedure known as radical lymph node surgery is often performed. This surgery involves the removal of these affected lymph nodes to prevent the cancer from spreading further. While this procedure is a key part of treating early stages of cancer that has reached the lymph nodes, it comes with significant risks and side effects. Patients undergoing radical lymph node surgery often experience complications, such as infections or poor wound healing. Additionally, they might develop lymphoedema, a condition where fluid builds up in the tissues, leading to swelling, usually in the legs or groin area. This can be a long-term issue that significantly impacts the patient’s quality of life.
Surgery alone is often not curative in cases where a patient’s cancer has extensive LN involvement. Currently, the benefits of adjuvant treatments remain uncertain and multimodal treatment approaches with (neo)adjuvant chemotherapy and/or radiotherapy are often considered for patients with extensive disease.
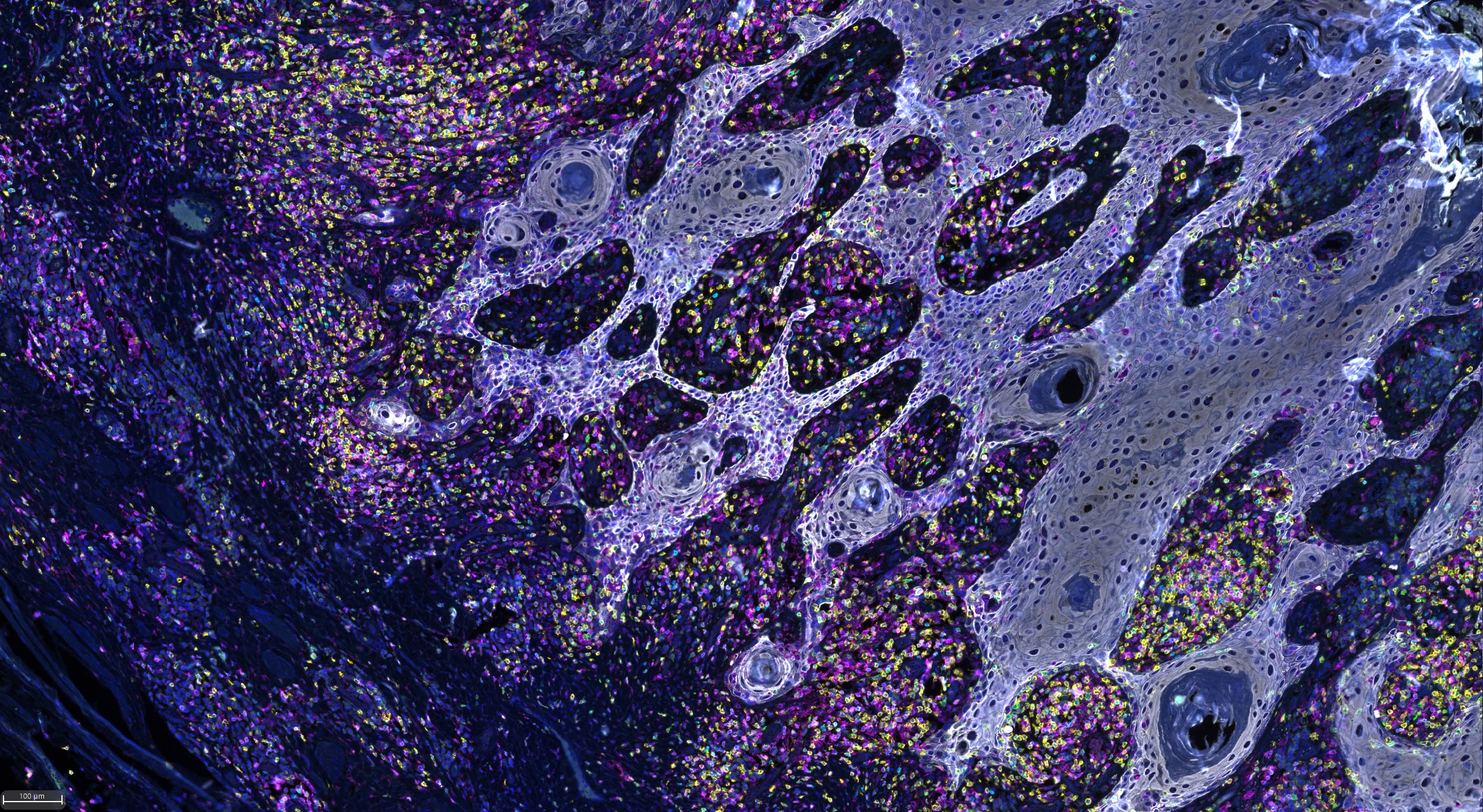
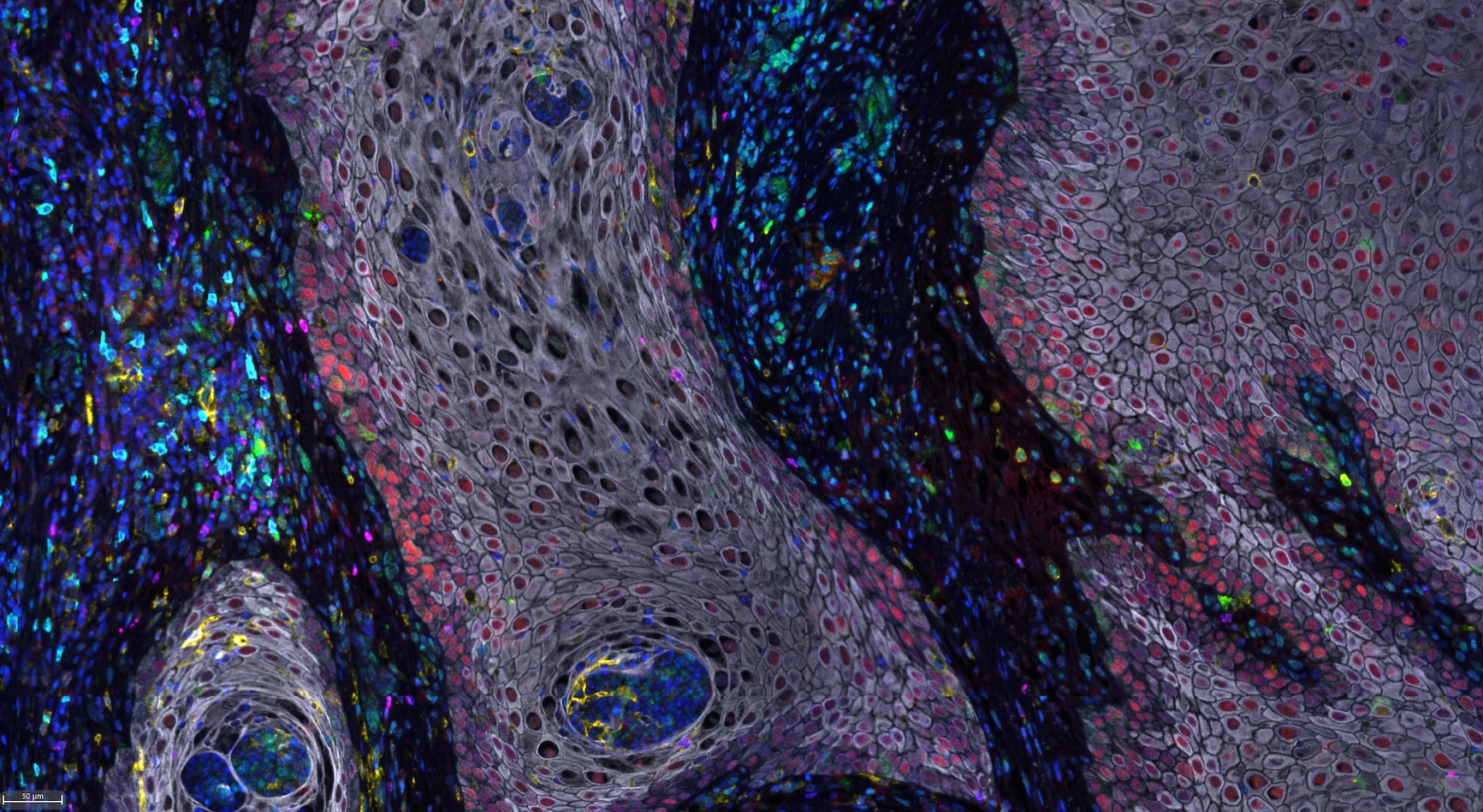
Stained Penile Cancer cells under the microscope
The Manchester solution
The Manchester team, alongside their international colleagues, set out to assess the clinical effectiveness of treatment options available for the management of inguinal and pelvic lymphadenopathy in men with penile cancer, with Dr Ashwin Sachdeva leading on the review article.
They systematically reviewed evidence of the clinical effectiveness of a series of approaches for the management of LN-positive penile cancer. The primary outcome here that the team were assessing was the five-year overall survival.
The team screened almost three and a half thousand abstracts and found just over 100 studies based on approximately 10,000 patients over the past 30 years. Given the rarity of this condition, most studies were observational or case series with only two randomised control trials identified.
In 2002, the NHS was one of the first healthcare systems in the world to concentrate the care of patients with penile cancer into specialist centres around the country (known as ‘supra-regional centres). These centres are specifically setup to provide the latest diagnostic and treatment options, supported by experienced staff and ancillary services like psychological support, lymphoedema services and support groups. They also work closely with charitable organisations such as ORCHID and Maggie’s which have excellent online resources and support services for men worried about penile cancer or are undergoing treatment. This model of care has been shown to improve outcomes in this group of patients including:
- Increased use of penile sparing surgery
- Accurate and appropriate assessment
- Management of lymph nodes
- Pathological assessment and improved survival
In England, there are a total of nine expert centres. Despite centralisation these centres have never been formally linked, which is a significant barrier to multicentre collaborative research, essential in rare diseases. The team at The Christie are working on addressing this need by working with partner organisations across the UK to establish the United Kingdom Penile Cancer Network UK (UK-PeCaN). UK-PeCaN will bring together units and PPV to share best practice and promote awareness and research in this group of patients. It will also look to use real world multicentre data to answer some of the most difficult and pressing questions in this underrepresented group of men.
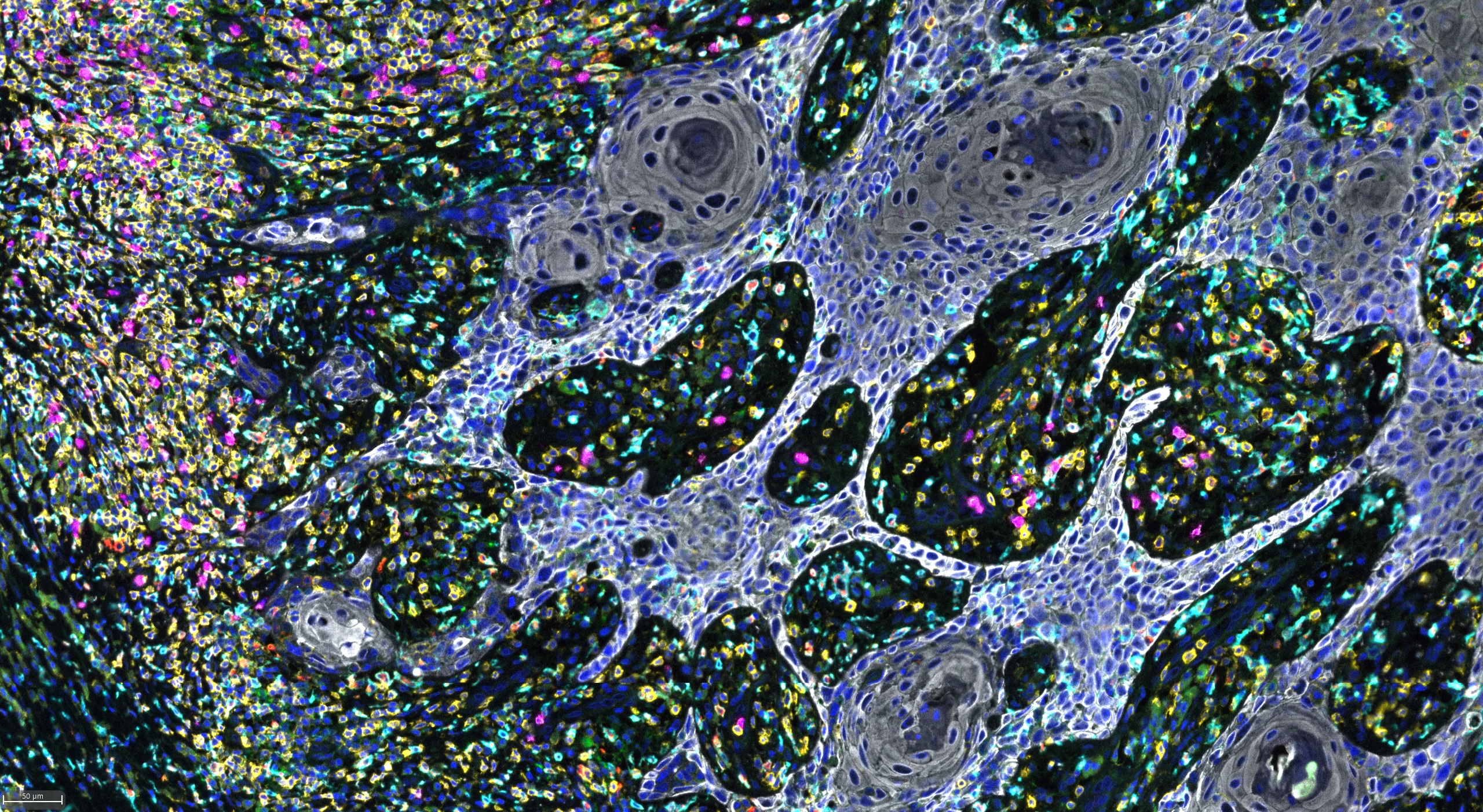
Stained Penile Cancer cells under the microscope
Treatment Conclusions
The systematic review concluded that the spread of penile cancer to the lymph nodes is best managed with surgery, when technically feasible, which both improves patient survival and has a curative potential. It was also found that additional treatment including radiotherapy and/or chemotherapy may further improve patient survival in advanced stage disease. The team also noted that patients with penile cancer with lymph node involvement should be treated by a multidisciplinary team.
Surgical treatment remains the mainstay of treatment in Lymph Node-positive Penile Cancer and early use of lymph node dissection is associated with a much-improved disease specific survival. However, unresectable groin disease requires multimodal therapy, particularly in situations where the disease is categorised as N3 – meaning the cancer has spread to lymph node(s) in one or both sides of the pelvis OR the cancer cells in a nearby lymph node have grown into surrounding tissues – and in this setting, adjuvant chemotherapy and adjuvant radiotherapy should be considered.)
This review concluded that given the rarity of penile cancer, there is a reasonably poor evidence base, but currently, this review offers the best literature summary to help clinicians understand the various nuances of the studies. The review has since helped inform current clinical decision making and has been used to develop these updated 2023 EAU-ASCO penile cancer guidelines.
The change in policy
Dr Ashwin Sachdeva and Dr Luke McGuiness were awarded the European Urology IMPACT Award for their article on “Management of Lymph Node-positive penile cancer: A Systematic Review” which was recognised as the most influential work in the March 2024 issue.
“We extend our heartfelt congratulations on this remarkable accomplishment and express our gratitude for the significant contribution they have made to our journal.” ~ Professor Alberto Briganti, Editor-in-Chief, European Urology
The previous guidelines did not recommend adjuvant radiotherapy, however based on the findings from this review, the 2023 guidelines recommend that patients with pN2 (metastasis in more than two unilateral inguinal nodes or bilateral inguinal lymph nodes) or pN3 (metastasis in pelvic lymph node(s), unilateral or bilateral or extra nodal extension of regional lymph node metastasis) should be offered adjuvant radiotherapy. The evidence accrued from the systematic review informed the process for developing the 2023 EAU-American Society of Clinical Oncology guideline.
These guidelines have had a particular focus on survivor issues and the importance of counselling patients.
Next steps
Through the systematic review, findings unearthed disparities in the use of radiotherapy, chemotherapy and/or chemoradiotherapy (CRT) and highlighted the need for high-quality collaborative multinational studies in the future.
In addition, poor outcomes and toxicity associated with current therapeutic modalities underline the unmet need for novel approaches that are both effective and tolerable in patients with advanced LN disease.
The Manchester Penile cancer service is provided at The Christie NHS Foundation Trust and is one of the largest in the world covering a population of approximately 8.7 million across the Northwest. With all aspects of care provided on a single site and co-located with academic pathology, Experimental Cancer Medicine Team, the research teams located within the Oglesby Cancer Research Building and The Paterson Building and the Cancer Research UK National Biomarker Centre there is a unique opportunity to leverage Manchester specific expertise for the benefit of this underrepresented group. The team also have a strong Patient/ Partner Voice community that is accessed through a dedicated support group and links with patient facing charities.
Currently the team are working in the following areas:
Translational:
- Examining the differences in the tumour micro-environment in metastatic penile cancer
- CRUK funded study on human papillomavirus (HPV)-associated penile cancer morphology & evolutionary heterogeneity
- Developing HPV positive and negative PDX models
- Use of Biomarkers and novel technologies in penile cancer to improve selection of patients for further adjuvant treatments.
Clinical:
- Trial evaluating whether novel approaches can reduce treatment related morbidity (VELRAD)
- Trial evaluating minimally invasive diagnostic techniques (BRUCY)
- Patient related outcome measures (PROMS)
Acknowledgements
Christie Penile Cancer Clinical Team
EAU-ASCO penile cancer guidelines panel
Useful resourses
For more information about penile cancer and a list of common symptoms, please visit the NHS website at NHS Conditions – Penile Cancer.
The following resources have been provided:
Management of Lymph Node-positive Penile Cancer: A Systematic Review

