Blood Cancer Awareness Month: How Meeting Patients Deepened My Commitment to Research
Written by Florentia Mousoullou, Cancer Sciences PhD Student and Science Communication Ambassador
Blood Cancer Awareness Month
September is Blood Cancer Awareness Month, an opportunity to spotlight a group of cancers that, despite affecting millions worldwide, are often overlooked.
Blood cancer isn’t just one disease; it includes leukaemia, lymphoma, and myeloma, each with its own complexities and challenges. Unlike many other cancers, blood cancers don’t form lumps or tumours. Instead, they begin in the blood or bone marrow, disrupting how the body produces and uses blood cells.
These cancers can be harder to spot and understand, yet they’re more common than people may realise. In the UK, someone is diagnosed with blood cancer every 14 minutes. Blood Cancer Awareness Month is about raising awareness, supporting patients and families, and reminding people that behind every diagnosis is a person.
My Research and Why It Matters
As part of my PhD, I study a type of blood cancer called acute myeloid leukaemia (AML). AML is a fast-growing cancer that affects the bone marrow, which is essentially the ‘factory’ inside our bones that produces blood cells. In AML, this factory produces abnormal white blood cells that crowd out the bone marrow, leaving less space for healthy red blood cells, which are essential for carrying oxygen and helping blood to clot to stop bleeding.
My research focuses on how the immune system, especially a type of white blood cell called a T cell, responds to blood cancer and blood cancer treatments. T cells are like the body’s security guards, trained to spot and kill dangerous cells like cancer cells. However, in AML, both the cancer and the treatments, like chemotherapy and transplants, can significantly affect T cell function – impairing their ability to fight cancer.
My research looks at how T cells respond to treatment, especially after stem cell transplants, to understand how we might reprogramme T cells to effectively target and kill cancer cells. This approach to treatment is an example of immunotherapy. In simple terms, I study the ‘messaging’ between cancer and the immune system to help us find better ways to treat leukaemia and reduce the chances of it coming back.

Researchers looking at data on a laboratory computer
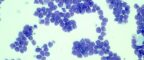
Acute Myeloid Leukaemia (AML) cells under a microscope
Behind the Scenes: My Hospital Experience
My research became personal when I spent time on the leukaemia ward at The Christie NHS Foundation Trust with my supervisor, Dr Mark Williams. Until then, my work mostly involved tissue samples and data in the lab. But in the hospital, I saw the real people who are affected by blood cancer and are the reason I carry out my research.
I joined clinical meetings where doctors, scientists, nurses, and pharmacists discussed each patient’s treatment plan in detail. These weren’t just medical checklists, they were thoughtful, complex conversations. Every decision mattered: how to balance the side effects of treatment, how to manage infections, how to prepare a patient for transplant, and how to support their mental health.
One moment I’ll never forget was when a doctor shared good news with a young patient and her mother burst into joyful tears – a reminder of how deeply parents carry the weight of their children’s illness.
That experience changed the way I approach my work. I now think of those families whenever I’m in the lab. I’m not just looking at cells under a microscope, I’m part of a wider effort to give people more time, better outcomes, and hopefully, a cure.
The first time I stepped onto the leukaemia ward, I wasn’t prepared for the resilience I’d see. One patient told me: “Every day I wake up is a win.“ That stuck with me.
Florentia Mousoullou
Cancer Sciences PhD Student and Science Communication Ambassador
Effective Treatment Options: The End Goal of Research
While blood cancers like AML are aggressive and complex, thanks to decades of research, treatments like stem cell transplants and better chemotherapy combinations provide patients with improved survival rates.
Other examples of AML treatments include CAR-T cell therapies (where T cells are genetically modified to attack cancer), and drugs that target genetic mutations found specifically in cancer cells.
Furthermore, NHS England now offers a targeted treatment called quizartinib for a specific genetic subtype of AML. This drug can be used alongside chemotherapy and continued for up to three years to help prevent relapse. Patients taking quizartinib have a median overall survival of nearly 32 months, compared to just over 15 months on standard treatment alone.
These strides across clinics, trials, and research, show how every piece of progress can ultimately help patients live longer, healthier lives.
How You Can Help — Even Without a Lab Coat
While researchers, doctors, and healthcare teams continue to make progress, our ability to improve the outcomes for people diagnosed with blood cancer also largely depends on public support.
Here are just a few ways you could help this Blood Cancer Awareness Month:
- Join the stem cell or bone marrow donor register through organisations like Anthony Nolan, DKMS, or NHS Blood and Transplant.
- Donate blood or platelets, especially for leukaemia patients undergoing chemotherapy or transplants, who often rely on regular transfusions.
- Support charities like Leukaemia UK, Blood Cancer UK, or Leukaemia Care, who fund research, support patients and families, and campaign for better treatment access.
- Talk about blood cancer. Sharing information, learning the signs and symptoms, or simply being aware of what patients go through can help to raise awareness of these often invisible diseases.
Why Blood Cancer Awareness Month Matters
As a scientist, I’m driven by curiosity. But as someone who’s met leukaemia patients and their families, I’m also driven by the hope that my research, and the work of so many others, can make cancer more treatable.
Every small discovery in the lab, every clinical trial, every moment of joy on a hospital ward brings us one step closer to better outcomes and, one day, a cure for blood cancer.

