MCRC Blog

MCRC Blog
23/09/2025
Faces of Leadership: Black Scientists Shaping Cancer Research and Care
This Black History Month, we celebrate Black leaders at the Manchester Cancer Research Centre, highlighting their proudest moments, lessons learned, and hopes for the future.
MCRC Blog
20/08/2025
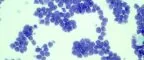
Blood Cancer Awareness Month: How Meeting Patients Deepened My Commitment to Research
September is Blood Cancer Awareness Month, an opportunity to spotlight a group of cancers that, despite affecting millions worldwide, are often overlooked.
MCRC Blog
13/08/2025
The 18th International PhD Student Cancer Conference Comes to Manchester
From 11–13 June 2025, The University of Manchester became a vibrant hub for early-career cancer research. Hundreds of PhD students and young scientists from across Europe came together to share their work, challenge ideas, and build a community that stretches far beyond the lab.
MCRC Blog
25/07/2025
Narrative Therapy for Trust-Building in Research
MCRC Blog
18/07/2025
Navigating Brain Tumour Diagnosis: Innovations and Strategies Symposium
On 2nd July 2025, leading experts in neuro-oncology gathered at the Pendulum Hotel in Manchester for the second annual Navigating Brain Tumour Diagnosis Symposium.
MCRC Blog
03/07/2025
Connect, Create and Unite: Lung Health Equity Workshop
MCRC Blog
17/06/2025
From Lab to Stage: Tips for Effective Research Presentations as a PhD Student
At a recent School of Medical Sciences Cross-Divisional Seminar, PhD students from various disciplines presented their work. PhD Cancer Sciences and Science Communications Ambassador, Florentia Mousoullou, asked three PhD students some key questions to try and shed light on the challenges and benefits of sharing research.
MCRC Blog
12/06/2025
‘Unseen Unheard’: The untold breast cancer stories of underserved Black women in the UK
MCRC Blog
12/06/2025
Global Collaboration in Action: Manchester at the STARS21 Summit
In May 2025, a group of early-career researchers from the Manchester Cancer Research Centre and The Christie NHS Foundation Trust travelled to Toronto, Canada, for the final gathering of the STARS21 programme – an inspiring international initiative shaping the future of radiation oncology.

MCRC Blog
29/05/2025
Manchester researchers present at AACR 2025
MCRC Blog
13/05/2025
Ca-PRI 2025: A Global Gathering on Cancer Innovation, Inequality, and Interdisciplinary Care
On 29–30 April 2025, more than 250 delegates from around the globe gathered at The Lowry in Salford, Manchester for the Cancer in Primary Care Research International (Ca-PRI) Conference 2025.
MCRC Blog
12/05/2025